What we know about how to avoid early-onset dementia, a rare Alzheimer's variant, and breaking new research
Why do some people develop dementia before age 65 while most clear that birthday without cognitive changes?
Risk factors include both lifestyle choices and other, prior health conditions, breaking research shows.
The study, cited in Jama Neurology, indicates that specific genes and previous strokes could yield young-onset dementia. But so too could social isolation, not getting enough sun, or too much alcohol.
Those experiencing hearing loss may also be at risk. This finding aligns with another, separate study out of the University of Southern Denmark Faculty of Health Sciences, which indicates auditory difficulties increase dementia risk approximately 7%.
While that report doesn’t mention early-onset specifically, officials said: “People who are hard of hearing spend more energy listening. That energy comes at the expense of other cognitive functions. Cognitive functions are the mental processes in the brain that enable us to think and solve problems, among other things.”
A University of California at San Francisco study found that a specific form of dementia — posterior cortical atrophy, an Alzheimer’s variant — usually manifests sooner than age 65, although diagnosis typically takes four years to achieve.
The earliest symptoms usually appear around age 59, and they are often vision-related, researchers say. Still, despite the difficulties with depth perception and discerning what is and isn’t moving, an eye exam won’t show any issues, UCSF officials state.
“Most patients see their optometrist when they start experiencing visual symptoms and may be referred to an ophthalmologist who may also fail to recognize PCA,” said study co-author Marianne Chapleau in a statement.
The sooner someone learns they are dealing with PCA, however, the sooner they can investigate whether it makes sense to try the newly-FDA-approved lecanemab, which scrubs the brain of amyloid plaque — an Alzheimer's Disease attribute — or another clinical trial.
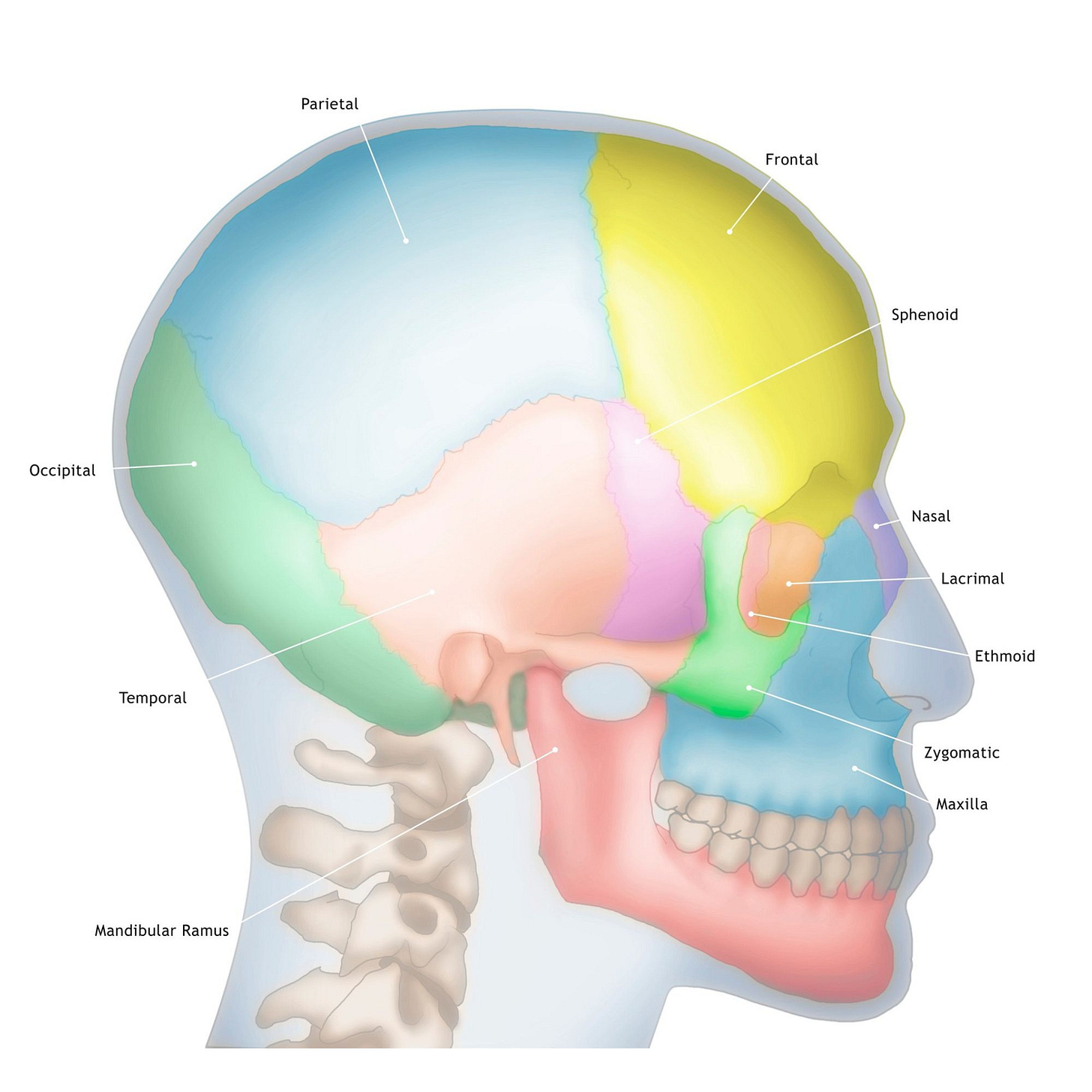
“Patients with PCA have more tau pathology in the posterior parts of the brain, involved in the processing of visuospatial information, compared to those with other presentations of Alzheimer’s,” said Renaud La Joie, another co-first study author. “This might make them better suited to anti-tau therapies.”
Such considerations highlight the need for earlier Alzheimer’s detection, and recently-published research indicates how that vision might soon become a reality.
The new study points to a specific blood biomarker test that can determine a brain’s amyloid and tau load with great precision.
“These accuracies were significantly higher than other plasma biomarker combinations and equivalent to cerebrospinal fluid (CSF) biomarkers,” Alzpath officials said in a statement.
This test scans for a biomarker known as phosphorylated tau at threonine 217, or p-tau217, which helps researchers discern whether a patient is dealing with Alzheimer’s or a different disease, the study authors say.
“A robust and accurate blood-based biomarker would enable a more comprehensive assessment of cognitive impairment in settings where advanced testing is limited,” the authors write for JAMA Neurology. “Therefore, use of a blood biomarker is intended to enhance an early and precise Alzheimer’s Disease diagnosis, leading to improved patient management and, ultimately, timely access to disease-modifying therapies.”
And there are so many new therapies to explore.
Neurosurgeon Ali Rezai has been experimenting with targeted ultrasound to treat Alzheimer’s, addiction, and other brain disorders, and his early findings offer patients hope.
“There’s no skin cutting. There’s no opening the skull. So it is brain surgery without cutting the skin,” he said in a 60 Minutes interview.
The procedure involves an expensive ultrasound helmet, a dosage of a plaque-stripping drug, a drip of small bubbles, and almost a thousand ultrasound beams.
Dan Miller was in his 50s when his Alzheimer’s symptoms began and became one of three participants in the study.
“For me it was just, let’s do this. What do I have to lose?” he says.
Once a month, he received an aducanumab infusion followed by the ultrasound treatment. For that, he was outfitted with a fancy helmet and given a bubble infusion that, when vibrated by the ultrasound, opened his blood-brain barrier so the medication could more efficiently enter the brain.
The thought was that this would accelerate the drug’s effectiveness. Typically, infusion treatment takes a minimum of 18 months. The infusion-ultrasound cocktail was administered over six months and was 50% more effective in lightening amyloid load when compared to just the drug.
Rezai is now studying how he might apply this technique to reverse Alzheimer’s-related brain damage, he says.
“There’s no miracle cures here. It’s advancing medicine with calculated risks and pushing the frontiers,” he says.
Breaking study suggests link between Alzheimer’s and inflamed gut: Says University of Wisconsin professor: “We showed [that] people with Alzheimer’s disease have more gut inflammation, and among people with Alzheimer’s, when we looked at brain imaging, those with higher gut inflammation had higher levels of amyloid plaque accumulation in their brains.”
Jay Leno’s April 9 conservatorship hearing will determine whether he can take over his wife’s estate as she navigates dementia. According to the filing, Mavis has “progressively [been] losing capacity and orientation to space and time for several years,” and is “substantially unable to manage his or her financial resources.”